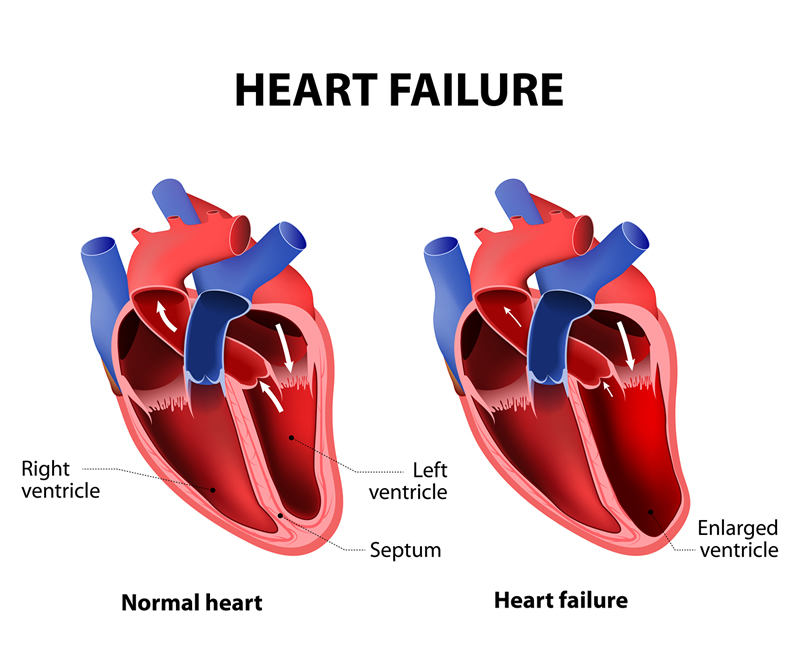
Congestive Heart Failure (CHF) is a chronic and progressive condition where the heart muscle is unable to pump blood effectively, resulting in an inadequate supply of oxygen and nutrients to the body’s tissues. This inefficiency causes blood to back up into the lungs and other parts of the body, leading to congestion and various health complications.
Table of Contents
Understanding Congestive Heart Failure
Congestive Heart Failure occurs when the heart muscle becomes too weak or stiff, impairing its ability to pump blood efficiently. This condition can develop gradually or suddenly and is often the result of other cardiovascular diseases. The term “congestive” refers to the buildup of fluid in the lungs and other tissues due to the heart’s diminished pumping ability.
Causes of Congestive Heart Failure
Several underlying conditions contribute to the development of CHF. Coronary artery disease, characterized by the narrowing or blockage of the coronary arteries, is the most common cause. This condition reduces blood flow to the heart muscle, leading to damage and weakening. High blood pressure, or hypertension, is another significant factor, as it forces the heart to work harder over time, eventually weakening the heart muscle.
Cardiomyopathy, a disease of the heart muscle itself, can result from various causes including genetic factors, chronic alcohol abuse, and certain infections. Heart valve diseases also play a role, as damaged valves force the heart to pump blood more forcefully. Additionally, arrhythmias, or abnormal heart rhythms, can impair the heart’s efficiency and lead to CHF. Diabetes often accompanies other risk factors such as hypertension and obesity, increasing the likelihood of CHF.
Symptoms of Congestive Heart Failure
The symptoms of CHF vary in severity and can develop either gradually or suddenly. Shortness of breath, especially during physical activity or while lying down, is a common symptom due to fluid accumulation in the lungs. Patients often experience fatigue and weakness because the heart’s reduced capacity to pump blood decreases oxygen delivery to tissues.
Swelling, or edema, particularly in the legs, ankles, and feet, is a hallmark of CHF caused by fluid buildup. A rapid or irregular heartbeat may occur as the heart tries to compensate for its reduced efficiency. Persistent coughing or wheezing can also be present due to lung congestion. Many patients experience an increased need to urinate at night, known as nocturia, resulting from fluid redistribution when lying down.
Diagnosis of Congestive Heart Failure
Diagnosing CHF involves a thorough medical history, physical examination, and various diagnostic tests. During the medical history and physical exam, doctors review symptoms, risk factors, and any history of heart disease. Physical exams may reveal signs such as lung congestion and abnormal heart sounds.
Blood tests can identify biomarkers like B-type natriuretic peptide (BNP), which is elevated in heart failure. An electrocardiogram (ECG) detects abnormalities in the heart’s electrical activity, while an echocardiogram, an ultrasound of the heart, evaluates heart structure and function. Chest X-rays can show heart enlargement and fluid in the lungs. A stress test assesses heart performance under exertion, providing insights into its functionality. Cardiac catheterization, an invasive procedure, helps identify coronary artery disease and other structural problems.
You May Also Read: What are the 7 signs of Rheumatoid Arthritis?
Treatment Options for Congestive Heart Failure
Managing CHF typically involves a combination of lifestyle changes, medications, and, in severe cases, surgical interventions. Lifestyle changes include dietary modifications such as reducing salt intake to prevent fluid buildup, engaging in regular exercise tailored to improve heart health, maintaining a healthy weight to reduce the heart’s workload, quitting smoking, and limiting alcohol and caffeine consumption.
Medications play a crucial role in managing CHF. ACE inhibitors and ARBs help relax blood vessels and lower blood pressure, reducing the heart’s workload. Beta-blockers slow the heart rate and decrease blood pressure, improving heart function. Diuretics, also known as water pills, help eliminate excess fluid, relieving symptoms of fluid retention. Aldosterone antagonists reduce fluid buildup and prevent worsening heart failure. Digitalis increases the strength of the heart’s contractions and helps control irregular heartbeats.
Surgical and medical procedures may be necessary for severe cases. Coronary bypass surgery improves blood flow to the heart muscle by bypassing blocked arteries. Heart valve repair or replacement restores normal blood flow by fixing damaged valves. Implantable cardioverter-defibrillators (ICDs) correct dangerous heart rhythms that can lead to sudden cardiac arrest. Cardiac resynchronization therapy (CRT) uses a specialized pacemaker to improve the timing of the heart’s contractions. A left ventricular assist device (LVAD) is a mechanical pump that supports heart function in severe heart failure. In end-stage heart failure, a heart transplant may be the best option.
Preventing Congestive Heart Failure
While not all cases of CHF can be prevented, adopting a heart-healthy lifestyle can significantly reduce the risk. Regular medical check-ups help detect and manage risk factors early. Proper management of chronic conditions like hypertension, diabetes, and high cholesterol is crucial. A diet low in saturated fats, trans fats, cholesterol, salt, and added sugars promotes heart health. Engaging in moderate physical activity most days of the week supports cardiovascular health. Avoiding tobacco and limiting alcohol consumption is fundamental in preventing heart disease.
Living with Congestive Heart Failure
Managing CHF is a lifelong commitment that involves regular medical care and lifestyle adjustments. Patients should work closely with their healthcare providers to monitor their condition and adapt their treatment plans as necessary. Support from family, friends, and patient support groups can also play a vital role in managing the emotional and psychological aspects of living with CHF.
Conclusion.
Congestive Heart Failure is a complex condition requiring comprehensive management. Understanding its causes, recognizing symptoms early, and adhering to prescribed treatments can improve the quality of life and outcomes for patients. By making informed lifestyle choices and staying engaged with healthcare providers, individuals with CHF can better manage their condition and maintain a higher standard of living.


Leave a Comment