Ulcerative colitis (UC) is a chronic inflammatory bowel disease (IBD) that primarily affects the colon and rectum. Understanding the leading cause of this debilitating condition is crucial for managing and potentially preventing it. This comprehensive article delves into the various factors contributing to ulcerative colitis, providing detailed insights into its etiology.
Table of Contents
Understanding Ulcerative Colitis
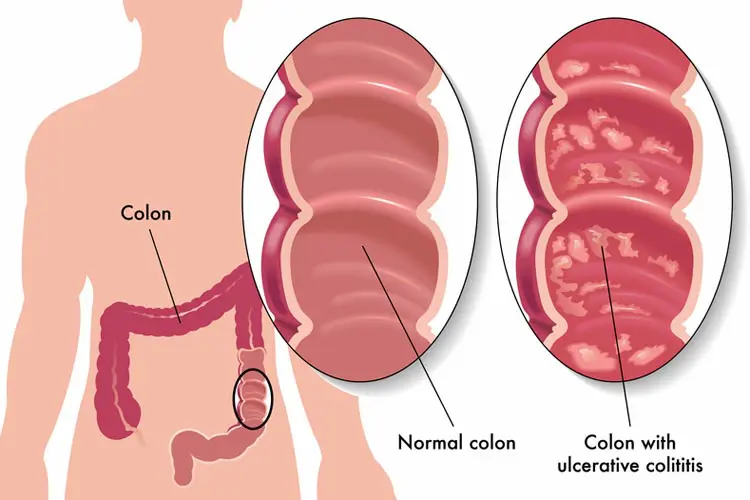
Ulcerative colitis is characterized by inflammation and ulceration of the inner lining of the colon and rectum. This inflammation often results in symptoms such as abdominal pain, diarrhea, rectal bleeding, and an urgent need to defecate. The exact cause of UC remains unknown, but research suggests a combination of genetic, environmental, immune system, and microbial factors.
Genetic Predisposition
The Role of Family History
One of the most significant risk factors for developing ulcerative colitis is a family history of the disease. Studies have shown that individuals with a first-degree relative (parent, sibling, or child) who has UC are at a significantly higher risk. This suggests a genetic predisposition to the disease. Numerous genes have been identified that may increase susceptibility to UC, particularly those involved in immune system regulation.
Genetic Mutations
Specific genetic mutations have been linked to ulcerative colitis. These mutations can affect the function of the immune system, leading to an inappropriate inflammatory response in the colon. Key genes implicated include those related to the regulation of the intestinal barrier, immune response, and microbial interactions.
Environmental Factors
Diet and Lifestyle
Environmental factors play a crucial role in the development and exacerbation of ulcerative colitis. Diet is a significant factor, with studies indicating that a high-fat, low-fiber diet may increase the risk of developing UC. Conversely, diets rich in fruits, vegetables, and whole grains are associated with a lower risk.
Lifestyle choices, such as smoking and physical activity, also impact UC risk. Interestingly, while smoking has been shown to exacerbate Crohn’s disease (another form of IBD), it may have a protective effect against ulcerative colitis. However, the exact mechanism behind this paradoxical effect remains unclear.
Stress and Psychological Factors
Stress and psychological factors are also believed to contribute to the onset and exacerbation of ulcerative colitis. While stress alone does not cause UC, it can trigger flare-ups in individuals with the condition. Chronic stress can lead to changes in the gut-brain axis, influencing gut motility, secretion, and permeability, thereby affecting the intestinal environment.
YOU MAY ALSO READ: What is Congestive Heart Failure Explain?
Immune System Dysfunction
Autoimmune Response
Ulcerative colitis is often considered an autoimmune disease. The immune system mistakenly targets the cells lining the colon, leading to chronic inflammation. This autoimmune response is thought to be triggered by a combination of genetic susceptibility and environmental factors.
Cytokine Imbalance
Cytokines are small proteins that play a critical role in cell signaling during immune responses. In individuals with UC, there is often an imbalance of pro-inflammatory and anti-inflammatory cytokines, leading to persistent inflammation. Targeting these cytokines with specific therapies has shown promise in managing UC symptoms.
Microbial Factors
Gut Microbiota Imbalance
The human gut is home to trillions of microorganisms, collectively known as the gut microbiota. These microbes play a crucial role in maintaining intestinal health. In individuals with ulcerative colitis, there is often a disruption in the balance of these microbial communities, known as dysbiosis.
Pathogenic Bacteria and Infections
Certain pathogenic bacteria and infections have been implicated in triggering UC. These pathogens can disrupt the normal gut flora, leading to an immune response that may contribute to the development of UC. Research is ongoing to identify specific microbial triggers and understand their mechanisms.
Potential Triggers and Risk Factors
Antibiotic Use
The use of antibiotics has been linked to an increased risk of developing ulcerative colitis. Antibiotics can alter the gut microbiota, potentially leading to dysbiosis and subsequent inflammation. This highlights the importance of cautious and judicious use of antibiotics, especially in individuals with a family history of IBD.
NSAIDs and Other Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to treat pain and inflammation. However, these medications can irritate the gastrointestinal tract and have been associated with the onset of UC. Other medications, such as oral contraceptives and certain immunosuppressants, may also influence UC risk.
Hormonal Factors
Hormonal changes, particularly those related to the menstrual cycle and pregnancy, can influence UC symptoms. Some women report worsening symptoms during menstruation or after childbirth, suggesting that hormonal fluctuations may play a role in disease activity.
Current Research and Future Directions
Advances in Genetic Research
Ongoing research aims to identify additional genetic markers associated with ulcerative colitis. Understanding these genetic factors can lead to better diagnostic tools and personalized treatments, potentially reducing the incidence and severity of the disease.
Microbiome Therapies
Therapies targeting the gut microbiome, such as probiotics and fecal microbiota transplantation (FMT), are being explored as potential treatments for UC. These therapies aim to restore a healthy microbial balance in the gut, reducing inflammation and improving symptoms.
Novel Immunotherapies
New immunotherapies are being developed to target specific components of the immune system involved in UC. These therapies, including biologic drugs and small molecule inhibitors, offer hope for more effective and targeted treatment options with fewer side effects.
Conclusion.
Ulcerative colitis is a complex disease with multiple contributing factors, including genetic predisposition, environmental influences, immune system dysfunction, and microbial imbalances. While the exact cause remains elusive, advances in research continue to improve our understanding of this condition. By addressing these various factors, we can develop more effective prevention and treatment strategies, ultimately improving the quality of life for individuals with ulcerative colitis.


Leave a Comment