Table of Contents
What is the Meaning of Clinical Depression?
Clinical depression, also known as major depressive disorder (MDD), is a severe form of depression that goes beyond the typical feelings of sadness or low mood. It is a complex mental health condition that affects a person’s emotions, thoughts, and behaviors, and it can significantly impair daily functioning. Understanding clinical depression involves exploring its symptoms, causes, diagnosis, and treatment options.
Symptoms of Clinical Depression
Clinical depression manifests in a variety of symptoms that persist for at least two weeks. These symptoms can be categorized into emotional, cognitive, and physical domains.
Emotional Symptoms
People with clinical depression often experience profound feelings of sadness, hopelessness, and emptiness. These emotional symptoms are persistent and not necessarily linked to specific events or situations. Other emotional symptoms include:
- Loss of interest or pleasure in activities once enjoyed, known as anhedonia.
- Feelings of worthlessness or excessive guilt.
- Irritability or frustration over minor matters.
- Persistent anxiety or agitation.
Cognitive Symptoms
Cognitive symptoms affect how individuals think and process information. Common cognitive symptoms include:
- Difficulty concentrating, making decisions, or remembering information.
- Pessimistic outlook on life and future.
- Recurrent thoughts of death or suicide, which require immediate attention.
Physical Symptoms
Clinical depression also has a significant impact on the body. Physical symptoms include:
- Changes in appetite lead to significant weight loss or gain.
- Sleep disturbances, such as insomnia or hypersomnia.
- Fatigue or low energy even with adequate rest.
- Slowed speech and movements, or conversely, restlessness and hyperactivity.
Causes of Clinical Depression
The causes of clinical depression are multifaceted and can be broadly categorized into genetic, biological, environmental, and psychological factors.
Genetic Factors
Research indicates that clinical depression can run in families, suggesting a genetic predisposition. Individuals with a family history of depression are at a higher risk of developing the condition themselves.
Biological Factors
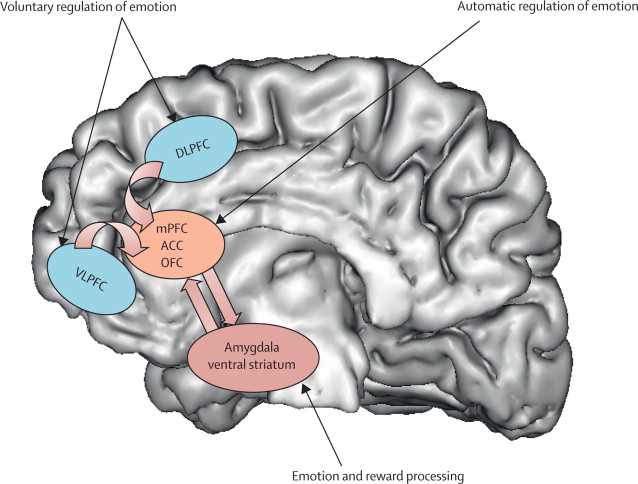
Biological factors include abnormalities in brain chemistry and function. Neurotransmitters like serotonin, norepinephrine, and dopamine play a crucial role in mood regulation. Imbalances in these chemicals can contribute to the development of depression. Additionally, hormonal changes, particularly those involving the hypothalamic-pituitary-adrenal (HPA) axis, have been linked to depression.
Environmental Factors
Environmental stressors, such as traumatic events, loss of a loved one, financial difficulties, or chronic illness, can trigger or exacerbate clinical depression. Social isolation and lack of support systems also play a significant role.
Psychological Factors
Personality traits, such as low self-esteem, perfectionism, and a tendency toward negative thinking, can increase vulnerability to depression. Furthermore, individuals with a history of other mental health conditions, such as anxiety disorders, are at a higher risk.
YOU MAY ALSO READ: What is a Parasite Cleanse?
Diagnosis of Clinical Depression
Diagnosing clinical depression involves a comprehensive assessment by a healthcare professional. This process includes:
Clinical Interview
A detailed clinical interview is conducted to understand the individual’s symptoms, medical history, and family history of mental health conditions. The healthcare provider may use standardized questionnaires, such as the Hamilton Depression Rating Scale (HDRS) or the Patient Health Questionnaire-9 (PHQ-9), to assess the severity of depression.
Physical Examination
A physical examination helps rule out any underlying medical conditions that may mimic depressive symptoms. Conditions like thyroid disorders, vitamin deficiencies, and neurological diseases need to be excluded.
Diagnostic Criteria
Clinical depression is diagnosed based on criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). The DSM-5 criteria include the presence of at least five of the following symptoms over two weeks, with at least one of the symptoms being either depressed mood or loss of interest/pleasure:
- Depressed mood most of the day, nearly every day.
- Markedly diminished interest or pleasure in all, or almost all, activities.
- Significant weight loss when not dieting or weight gain.
- Insomnia or hypersomnia.
- Psychomotor agitation or retardation.
- Fatigue or loss of energy.
- Feelings of worthlessness or excessive guilt.
- Diminished ability to think or concentrate.
- Recurrent thoughts of death or suicide.
Treatment Options for Clinical Depression
Treatment for clinical depression is tailored to the individual’s specific needs and often involves a combination of therapies.
Psychotherapy
Psychotherapy, or talk therapy, is an effective treatment for clinical depression. Different types of psychotherapy include:
Cognitive Behavioral Therapy (CBT)
CBT helps individuals identify and change negative thought patterns and behaviors that contribute to depression. It is a structured, goal-oriented therapy that focuses on problem-solving.
Interpersonal Therapy (IPT)
IPT addresses interpersonal issues and aims to improve communication skills and relationships, which can alleviate depressive symptoms.
Psychodynamic Therapy
Psychodynamic therapy explores unconscious processes and unresolved conflicts from the past that may be influencing current behavior and emotions.
Medication
Antidepressant medications can help correct chemical imbalances in the brain. Common classes of antidepressants include:
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are often the first-line treatment due to their efficacy and relatively mild side effects. Examples include fluoxetine, sertraline, and citalopram.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs, such as venlafaxine and duloxetine, target both serotonin and norepinephrine to alleviate depressive symptoms.
Tricyclic Antidepressants (TCAs)
TCAs, like amitriptyline and nortriptyline, are effective but have more side effects, so they are usually prescribed when other medications are not effective.
Monoamine Oxidase Inhibitors (MAOIs)
MAOIs, such as phenelzine and tranylcypromine, are typically used as a last resort due to their potential for severe side effects and dietary restrictions.
Lifestyle Changes
Incorporating healthy lifestyle changes can significantly impact the management of clinical depression. These changes include:
Regular Exercise
Physical activity boosts endorphins and serotonin levels, which can improve mood and energy levels.
Healthy Diet
A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support overall mental health.
Adequate Sleep
Maintaining a regular sleep schedule and ensuring sufficient rest is crucial for emotional well-being.
Support Systems
Building a strong support system through family, friends, or support groups provides emotional support and reduces feelings of isolation.
Alternative Therapies
Some individuals may benefit from alternative therapies such as acupuncture, meditation, or yoga, which can complement traditional treatments.
Conclusion.
Clinical depression is a complex and debilitating condition that requires a comprehensive approach to treatment. By understanding its symptoms, causes, diagnosis, and treatment options, individuals can better manage their condition and work toward recovery. Early intervention and ongoing support are crucial in improving outcomes for those affected by clinical depression.


Leave a Comment