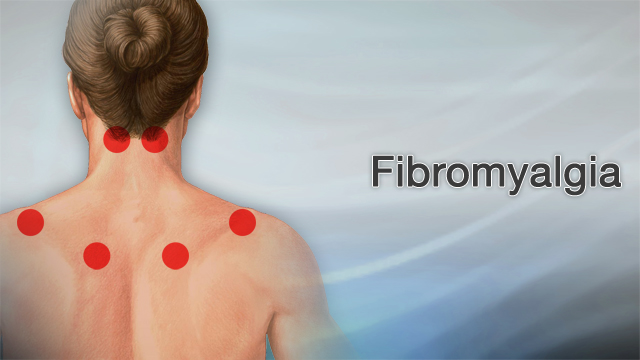
What is the Main Cause of Fibromyalgia?
Fibromyalgia is a complex and often misunderstood disorder characterized by widespread musculoskeletal pain accompanied by fatigue, sleep, memory, and mood issues. While its exact cause remains elusive, ongoing research has provided valuable insights into potential triggers and contributing factors. In this comprehensive article, we delve into the main causes of fibromyalgia, examining genetic, environmental, and psychological factors that play a crucial role in its development.
Table of Contents
Genetic Predisposition: A Significant Contributor
Research has shown that genetic factors play a significant role in the development of fibromyalgia. Studies indicate that fibromyalgia tends to run in families, suggesting a hereditary component. Certain genetic mutations may influence the way pain signals are processed in the brain, making individuals more susceptible to developing the condition. Genetic variations in genes related to serotonin, dopamine, and catecholamine pathways have been implicated in fibromyalgia, highlighting the importance of genetic predisposition.
Central Nervous System Abnormalities
Fibromyalgia is often associated with abnormalities in the central nervous system (CNS). Patients with fibromyalgia exhibit heightened sensitivity to pain, known as central sensitization. This phenomenon involves an increased response to pain signals in the brain and spinal cord. Neurotransmitter imbalances, particularly involving serotonin and norepinephrine, are believed to contribute to this heightened pain perception. Additionally, functional MRI studies have shown altered brain activity in regions responsible for pain processing in fibromyalgia patients.
Environmental Triggers and Stress
Environmental factors and stress are significant contributors to the onset and exacerbation of fibromyalgia symptoms. Traumatic events, such as accidents, surgeries, or infections, can trigger the development of fibromyalgia in predisposed individuals. Chronic stress, both physical and emotional, can also play a pivotal role. Stress activates the hypothalamic-pituitary-adrenal (HPA) axis, leading to an overproduction of cortisol, which may disrupt the body’s pain regulation mechanisms. Prolonged exposure to stress can further exacerbate symptoms and perpetuate the cycle of pain and fatigue.
Sleep Disturbances
Sleep disturbances are both a symptom and a contributing factor to fibromyalgia. Many individuals with fibromyalgia experience non-restorative sleep, characterized by frequent awakenings and difficulty reaching deep, restorative stages of sleep. This lack of quality sleep can exacerbate pain and fatigue, creating a vicious cycle. Research suggests that disruptions in the body’s natural sleep-wake cycle can affect the central nervous system’s ability to regulate pain, further highlighting the importance of addressing sleep issues in fibromyalgia management.
YOU MAY ALSO READ: What If LDL Cholesterol Is High?
Psychological Factors and Mental Health
Psychological factors, including anxiety, depression, and emotional trauma, are closely linked to fibromyalgia. The brain’s response to emotional stress and trauma can influence pain perception and sensitivity. Individuals with a history of psychological trauma or chronic mental health conditions may have an increased risk of developing fibromyalgia. Furthermore, the burden of living with chronic pain and fatigue can contribute to the development of anxiety and depression, creating a complex interplay between psychological and physical symptoms.
Immune System Dysfunction
Emerging research suggests that immune system dysfunction may play a role in fibromyalgia. Some studies have identified abnormal immune responses in fibromyalgia patients, including elevated levels of pro-inflammatory cytokines. These cytokines can contribute to chronic inflammation and pain. Additionally, autoimmune conditions, such as rheumatoid arthritis and lupus, are often comorbid with fibromyalgia, indicating a potential link between immune system abnormalities and the disorder.
Hormonal Imbalances
Hormonal imbalances, particularly involving thyroid hormones and sex hormones, have been implicated in fibromyalgia. Thyroid dysfunction, such as hypothyroidism, can mimic or exacerbate fibromyalgia symptoms. Women are disproportionately affected by fibromyalgia, leading researchers to investigate the role of hormonal fluctuations in the development and severity of the condition. Estrogen and progesterone levels may influence pain perception and sensitivity, further contributing to the gender disparity observed in fibromyalgia prevalence.

Gut Health and Fibromyalgia
Recent studies have explored the connection between gut health and fibromyalgia. The gut-brain axis, a bidirectional communication network between the gastrointestinal tract and the central nervous system, plays a crucial role in maintaining overall health. Dysbiosis, an imbalance in the gut microbiota, has been linked to chronic pain conditions, including fibromyalgia. Gastrointestinal symptoms, such as irritable bowel syndrome (IBS), are common in fibromyalgia patients, suggesting a potential link between gut health and the disorder.
Lifestyle Factors and Fibromyalgia
Certain lifestyle factors can influence the development and progression of fibromyalgia. Sedentary behavior, poor diet, and lack of physical activity can contribute to the worsening of symptoms. Conversely, regular exercise and a balanced diet rich in anti-inflammatory foods can help manage fibromyalgia symptoms. Mind-body practices such as yoga, meditation, and tai chi have shown promise in reducing pain and improving quality of life for fibromyalgia patients.
Conclusion.
In conclusion, fibromyalgia is a multifaceted disorder with no single cause. Genetic predisposition, central nervous system abnormalities, environmental triggers, sleep disturbances, psychological factors, immune system dysfunction, hormonal imbalances, gut health, and lifestyle factors all contribute to its development and severity. Understanding these complex interactions is crucial for developing effective treatment strategies and improving the quality of life for individuals living with fibromyalgia.